Emergent Supply Chain Challenges for Deployment of the COVID19 Vaccine: Saving the Commons
As we enter into the early stages of the second wave of COVID cases, hospitals and public health administrators are worried about the new influx of cases that will arrive before the development and deployment of COVID vaccines in 2021. During this period, we are continuing to experience a shortage of PPE’s, and multiple healthcare providers, distributors, and Group Purchasing Organizations are struggling to source masks, gowns, and gloves. Simultaneously, shortages of reagents, plastic trays, test kits, and pipettes are continuing to be experienced, limiting the needed tests that will enable safe return to schools and places of work.
One thing we’ve learned since the early days of the COVID crisis is the importance of advance planning and preparedness. In an earlier paper we wrote in the Millbank Journal that was built upon our experiences working on the front lines of the healthcare PPE response, we developed the concept of the “tragedy of the commons”, which occurred due to a lack of advance planning. Our research, focusing on common products needed in times of stress, focuses on both institutional arrangements – especially design and governance of the national stockpile, which as we will see, is intended to be a commons for the nation.
The idea of common goods is now recognized as expansive to other areas and is well-suited to our focus on the issues of design, development and governance for key critical medical supplies as common resources. The importance of these features has been well known as has the role of the public sector. As we look forward with hope to the deployment of the vaccine, it is imperative that we consider the possible supply chain issues that could arise, and learn from the mistakes made during the first wave of the COVID response.
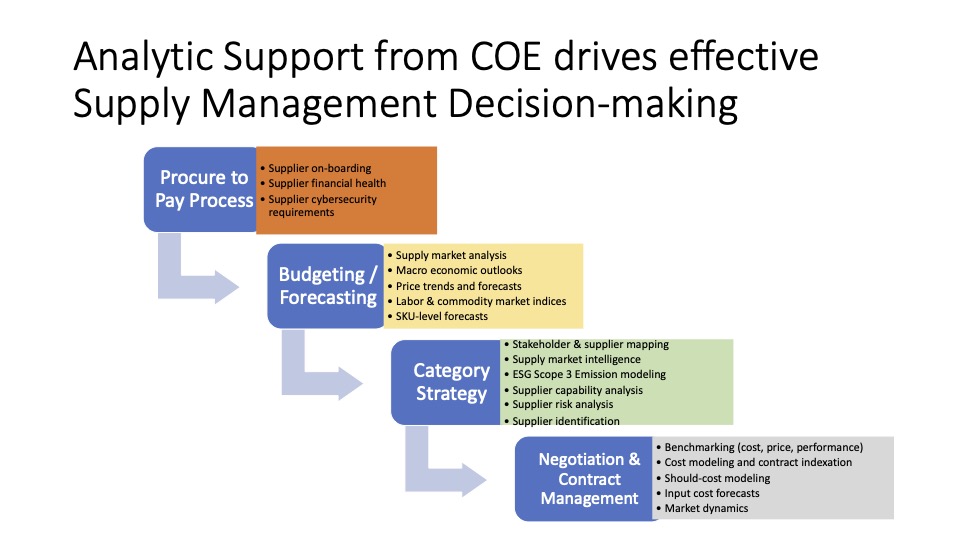
In the following blog, I’d like to share some insights into the potential problems that exist in the vaccine supply chain. This information relies on our personal observations, discussions, insights obtained from media, relying on our deep network of individuals who are actively involved in the COVID response within both the private and public sector. Supply chains cross both of these sectors, and many of the challenges we envision will occur through the inadequate interface that exists between these two entities. We employ a framework developed by the Supply Chain Council, the Supply Chain Operating Reference (SCOR) model, and classify the major challenges that exist in each area. We also offer potential solutions to address these challenges, in the hopes that public healthcare policy makers can think through these issues in their planning documents. The new administration has an opportunity to really make a difference here.
Vaccine Deployment Issues
The CDC has established a planning document that identifies three phases of distribution that will occur once a vaccine (or vaccines) are approved.
Phase 1 – Potentially Limited Doses Available (limited to first responders)
Phase 2 – Large Number of Doses Available (Critical Populations)
Phase 3 – Continued Vaccination, Shift to Routine Strategy.
Within this framework, the CDC notes that the only anticipated supply shortage might occur during Phase 1, during the initial growth in demand for vaccinations, but assumes that “likely sufficient supply to meet demand” during Phase 2 and 3. This is an important issue, as the assumption that supply bottlenecks will be solved during this point may be a challenging issue indeed. Our view is that there will exist major issues not just with vaccine supply, but with distribution issues as well. We document these issues using the following SCOR framework of PLAN – SOURCE – MAKE – DELIVER – RETURN. Here are some of the potential roadblocks that exist.
PLAN
BARDA has estimated that 650 to 850 million syringes and needles will be needed, yet there are significant capacity limitations here that may exist. Our experience is that production capacity often needs to be booked a year in advance and must be committed to upfront. The total US capacity of syringes is estimated at 40M from RTI in 2020, 40M from RTI in 2021, and 140M from BD in 2020-2021.
In addition, planning requires monitoring of testing, and identification of how many tests have been administered. A control tower is needed to measure this, as well to record any adverse reactions that may occur during testing.
SOURCE
There many other significant bottlenecks that could arise during the deployment of a vaccine. These include stoppers, adjuvants, cold storage, lipids, and raw materials for syringes and stoppers. In particular, fill-finish capacity will be challenging to find on such a large scale, and there may be variation in the forecasts required to establish contracts with these third party contractors.
MAKE
Fill-finish capacity is required to meet the needs of the four or five emerging vaccines on the market, and industry experts are concerned that there is a bottleneck in the production of the brewing equipment that is needed to expand capacity, and that it may take 6 to 8 months to fill orders. The Department of Defense and BARDA have a contract with SiO2 Materials Science for plastic vials: 40 million in June, 80 million in September, and 120 million in November. These plastic vials have a microscopic glass coating, and according to SiO2, can be manufactured in a quarter of the time of glass vials. In March, SiO2 was producing only 14 million vials per year; it is unknown whether SiO2 hit its June production targetPfizer is retrofitting existing facilities, but investment is needed including Millipore Sigma and ThermoFisher Scientific. These companies need stainless steel tanks and disposable plastic bags for processing a vaccine.
DELIVER
Cold chain logistics capacity is limited, as there is little information known yet about which vaccines will emerge as the likely winners. There is also little information yet established about how allocation will be ensured to the different parties identified in the CDC Covid plan, and how the vaccines will be administered to the public (hospitals, doctor’s offices, pharmacies) and how the determination of whether a prioritized individual is verified.
RETURN
The collection and disposal of the syringes will be a massive task. How these will be disposed of is not yet a consideration, and the logistics for collection is also not well documented.
These challenges will need to be addressed in the weeks that follow, and the new administration will be an important part of ensuing that this occurs.