The Perilous State of Healthcare Supply Chains Today: How Did We End Up Here?
In my last couple of blogs, I spoke briefly about the current surge in demand for N95 masks, as well as the number of grocery stores that were experiencing severe shortages of paper products, hot dogs, and rice & beans…if only those were the only issues we had to worry about! Since then, I have been on a number of different calls all focused on a much greater issue of significant and real concern that Americans need to be worried about: the healthcare supply chain.
Several articles and news reports have begun to identify the nature of these critical shortages. Late last week I read the results of a recent University of Washington modeling study, that identified the nature of the shortages that we are likely going to see in the next several weeks. This included a lack of 64,000 hospital beds and 17,309 ICU beds, a shortage of 19,481 ventilators, and estimates of between 81,000 and 162,000 deaths as a result of these shortages in hospitals.
Several projects have sprung up in the face of the dire shortages of hospital supplies. One of these is the Covid Network, started up by the Helena Group. Its purpose is to answer the most critical questions facing those with the power to deliver aid: where are extra supplies (masks, globes, ventilators, hydroxychloroquine), or even doctors themselves, most needed now? And where will they be most needed tomorrow, next week and beyond?Helena’s goal is for the platform to be able to answer these questions using real-time data from hospitals, CDC information about the spread of the virus, census data on the concentration of at-risk populations (e.g. the elderly), and other relevant inputs. Like all of their COVID work, this platform will be offered completely free of charge through its non-profit arm. The shortage of hospital PPE, ventilators, and other components is shown by location, based on risk factors and local populations. The short-term picture, I’ll warn you, isn’t good. Hospitals in New York will be impacted first, but others throughout the country will be increasingly facing many shortages by mid-April to early May, when the peak is expected to occur. For this reason, stay indoors as much as possible – and also try not to get injured. You really don’t want to end up in the hospital ER full of suspected CoVid patients who haven’t been tested yet..Another problem, stated by a physician I interviewed this week, is that hospitals are not always being forthcoming about the shortages they are facing. They may be afraid that someone will be held accountable – when in fact, we are all accountable in this situation.
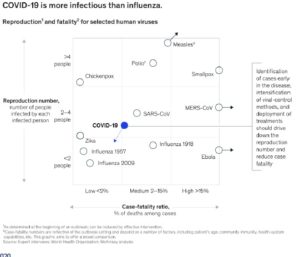 The lack of coronavirus testing kits is exacerbating the situation, as we don’t know who is sick and who isn’t, and the symptoms often take a week or more to show up. As shown in the chart to the left, Covid-19 appears both more deadly and contagious than other well known influenzas: a main cause though is the lack of a vaccine. The reproduction number is right around 2.6, (each sick person infects 2.6 other people on average), which means it is highly contagious, and is an incredibly robust virus, remaining on packages deliveries, surfaces, and in the air for significant periods of time. For this reason, it is spreading exponentially, and is proving to be difficult to address. This is why the contagion is so difficult to control, and also has resulted in such a high death rate…because we don’t have a vaccine.
The lack of coronavirus testing kits is exacerbating the situation, as we don’t know who is sick and who isn’t, and the symptoms often take a week or more to show up. As shown in the chart to the left, Covid-19 appears both more deadly and contagious than other well known influenzas: a main cause though is the lack of a vaccine. The reproduction number is right around 2.6, (each sick person infects 2.6 other people on average), which means it is highly contagious, and is an incredibly robust virus, remaining on packages deliveries, surfaces, and in the air for significant periods of time. For this reason, it is spreading exponentially, and is proving to be difficult to address. This is why the contagion is so difficult to control, and also has resulted in such a high death rate…because we don’t have a vaccine.
So, what about a remedy? Well, there is activity here too: There are roughly 35 organizations racing to create a vaccine, 4 have candidates in animal testing, and 1 started human trials. Some of these are utilizing and repurposing prior SARS candidates, given that there is an 80+ % overlap of genetic material with Sars-CoV-19. Antivirals slow the replication of the virus early on, or drugs that stop the cascade of illness, and there are some possibilities. There are currently 69 drugs identified as potentials, with 14 under investigation. Of course, it is faster to repurpose current drugs than develop new ones, but rigorous testing is required. This makes it difficult to obtain significant sample sizes for so many trials. All of these activities are going to take awhile to develop, and in the meantime, everyone is quarantined. The goal of doing so is to postpone the rush on hospitals – but the chances of getting the virus are pretty good – it’s just a matter of when, (not if).
This raises an important question: Why is the healthcare system so unprepared? During the last pandemic in 2010 (SARS), executives swore up and down that they wouldn’t let this happen again. And government bureaucrats also assured everyone that a strategic stockpile would be maintained. Nine years went by… and people somehow lost track of the impact of a major health epidemic sweeping the world. The problem today is that organizations forgot to replenish and prepare stockpiles for one of the world’s worst epidemics – one that is for the history books. This is a function of a couple of different factors.
Stockpiling supplies and/or creating redundant sources of supply is one of the most often cited strategies associated with pre-emergency planning. The cost of stockpiling is not insignificant, and requires an investment in products that go into inventory and which may or may not be utilized in the short term. Typical inventory holding costs are in the range of 18 percent to 25 percent of the value of a good on an annual basis, and include opportunity costs, storage, interest, insurance, shrinkage, and obsolescence. But executives aren’t rewarded for holding inventory, in fact it shows up as a penalty in the form of lower working capital…so guess what. Nobody stockpiled.
Stockpiling also occurs some serious business continuity planning. Questions executives need to ask themselves surrounding supply chain stockpiling of goods include the following:
• What types of supplies are required?
• What other types of redundancies can be identified (e.g., second source of supply, multiple transportation routes, etc.)?
• Who are the critical individuals requiring access to stockpiles?
• What is the right quantity of supply and redundancy?
• What is the relative cost of supply and redundancy?
In the current panic, nobody has answers to these questions, and there is no centralized task force that is planning and creating insights into how to deploy assets. Worse yet, there are few sources of supply market intelligence to identify where production of these goods is going to come from. Demand models (like the Helena group) are a good start, but without supply, such models are only going to predict a lot of shortages, but not offer any solutions! (The Supply Chain Resource Cooperative in collaboration with the College of Textiles is working on collecting market intelligence from various sources, to create a focal point for understanding what capacity and supply will look like. But it is very difficult – and a very fast moving situation…).
Stock-piling ahead of an actual pandemic is an important strategy, and is made even more critical given the length of time required to develop and distribute vaccines. The length of time to isolate a strain and develop a vaccine is often 6 months or longer, so hospitals and organizations should rely on other forms of prevention in the short term. Interviews with key experts also reveal that, once a vaccine is identified and isolated (which could take 6 to 12 months), the actual vaccine treatment requires two shots, spaced 21 days apart, which further lengthens the response time. More-mature organizations have developed sophisticated approaches to measuring and deploying stockpiles. As noted earlier, the costs of doing so are not insignificant. As such, a cost model to identify the different costs of stockpiling, relative to the lost wages and productivity associated with employee illness, was developed.
This brings up another important point lost on many executives since the last pandemic: how organizations value inventory, and where that inventory is located. Because so many healthcare products moved to China, which is now hoarding products for their own purposes to support their own possible second wave of coronavirus victims, hospitals are short of these products. It’s one thing to produce masks, but you still need raw materials. Ventilators is another issue – GM can’t just turn around and start producing them – it will take at least a month. This occurred because everyone wanted the “cheapest” product possible.
Why did this happen? Again, purchasing executives are generally rewarded on the basis of one major factor: buy it cheaper any where and any time you can. Price is all that manners. In short, it is part of the supply manager’s gestalt to continue to focus on a negotiated cost savings of 5 to 10% for logistics or purchase price, but not to strive for anything more. Such savings don’t amount to much when an entire month’s worth of orders is wiped off the books by the Brexit or trade deal increases tariffs by 25%. When the entire global economy shuts down for two or three months, and people start dying, then it becomes a lot more than a mistake. It becomes a catastrophe of the highest order. Meanwhile, organizations that have more tightly compressed supply chains with local suppliers are enjoying a significant benefit during the COVID crisis, and are no longer being held hostage to governments of another country. During a crisis, countries become very selfish, as illustrated by the hoarding of N95 masks and restrictions of exports by more than 27 countries. (When it comes to a pandemic, governments become surprisingly unwilling to collaborate and help one another out…it’s basically every man for himself..)
The future (post-CoVid) global economy is likely going to change forever after the dust has settled. Thousands of people will have died, and even for those who make it through, scarring of lung tissue can hamper their lives. The scary thing about this situation is that another coronavirus is possible. A recent study found that “…pandemic risk may be seasonal and predictable, with the accuracy of pre-pandemic and real-time risk assessments hinging on reliable seasonal influenza surveillance and precise estimates of the breadth and duration of heterosubtypic immunity.” What that means is that the cirus could indeed come back in a different form – but this time, hopefully we will be on the lookout for the early signs, and start to create strategic stockpiles to support hospitals and healthcare workers putting their lives on the line. The lack of healthcare products produced locally may also result in increased levels 0f domestic production, and a move to a more local supply base of critical products like ventilators, masks and PPE.
I wish I had a better upside story to tell here, but I think we are all learning about this as we go…everyone stay inside and stay safe.